Fitness
Specification curve analysis to identify heterogeneity in risk factors for dementia: findings from the UK Biobank – BMC Medicine

Through two specification curve analyses—one encompassing a comprehensive range of established dementia risk factors and the other focusing on a subset of particularly stable risk factors to study combinational effects—we identified heterogeneity in the risk for various dementia subtypes and across different age groups. Nonetheless, modifications in age categorization or demographic factors exerted negligible influence on the associations between risk determinants and dementia manifestations. Of particular significance were traumatic brain injury (TBI) and the APOE e4/e4 allele, which demonstrated consistent associations with all examined dementia subtypes across all analytical conditions. In contrast, risk factors such as diabetes exhibited variable correlations with diverse dementia outcomes. Furthermore, individuals with unattributed dementia participants displayed risk profiles that were analogous to those with definitive subtypes, transcending age delineations.
In this study, we included 450,707 participants from the UK Biobank with ages greater than 45 years old and divided them into two groups: midlife (45–65 years old) and late-life (greater than 65 years old). The midlife group consists of about 83% of all the participants. UK Biobank participants accrued 2710 all-cause dementia (44.5% female, about 0.6% of all UK Biobank participants), 1005 Alzheimer’s Disease (48.9% female), 539 vascular dementia (36.4% female), and 113 frontotemporal dementia (43.4% female) diagnoses during follow-up. There are 20%, 13%, 26.5%, and 12.4% of all-cause dementia, Alzheimer’s disease, frontotemporal dementia, and vascular dementia participants in the midlife group. The results from SCA analyses are summarized by the median ORs, their interquartile ranges (IQR), and the percentage of significant model outputs in Tables 1 and 2. The definitions we used to query the risk factors are shown in Additional file 2: Table S1. Details about the number of participants included for each risk factor among different age groups and prevalence can be found in Additional file 1: Figure S1 and Additional file 2: Table S2.
Specification curve analysis to illustrate analytic heterogeneity in different models
Our comprehensive specification curve analysis revealed significant findings regarding dementia risk factors. The comprehensive specifications consist of three categories of experimental variables to model the dementia subtypes as the outcome, outlined in Fig. 1. Out of 1445 models in Fig. 2, 716 showed statistically significant results (p
We presented the details of the comprehensive specifications of our models in Table 1. The age groups showed that more midlife participants contributed to large ORs than late-life participants. We did not observe distinguishable differences in estimates depending on covariate sets in any specifications. For the same risk factor (e.g., diabetes) under different model adjustments, the odds ratio varied. Diabetes had inconsistent associations in different age groups (midlife median OR 0.52 [0.37–0.96] and late-life median OR 1.86 [1.22–2.51]). On the other hand, most other risk factors had similar associations with dementia regardless of the age group evaluated. PM2.5 ORs differed based on analytic specification; for example, the top quintile has a midlife median OR 1.43 [1.15–1.45] and a late-life median OR 1.39 [1.29–1.49], which is higher compared to the second quintile (midlife median OR 1.10 [1.08–1.16] and late-life median OR 1.21 [1.19–1.23]).
The Lancet study’s risk factors had varying levels of robustness, with some showing smaller odds ratios (ORs) in the UK Biobank (Additional file 1: Figure S2). Traumatic brain injury (TBI) showed a median OR of 8.43 [7.19–10.58] for midlife and 8.29 [7.47–9.27] for the late-life group in both studies, with significant midlife OR difference. Depression ORs were higher in UK Biobank across all ages (midlife = 2.11 [2.04–2.32], late-life = 2.09 [1.89–2.25]), while hypertension ORs were higher in the Lancet but lower in UK Biobank (midlife = 1.69 [1.61–2.18], late-life: 2.37 [1.45–3.12]). No significant late-life risk factor differences were noted. Inconsistencies in excessive alcohol consumption and physical inactivity associations between studies may relate to UK Biobank’s smaller sample size, as shown in Additional file 2: Table S2. These disparities suggest population differences as a potential cause of heterogeneity in risk factor impacts. Furthermore, we are interested in studying the impacts of multiple risk factors in one model on the ORs.
Specification curve analyses highlight several robust risk factors in association with dementia outcomes
To test the robustness of six selected risk factors (TBI, APOE e4/e4, hypertension, diabetes, depression, and education) from the previous specification curve analyses, we executed 3912 multivariate logistic regression models with different combinations of the selected risk factors (while adjusting for age, gender, and ethnicity) (Fig. 3 and Table 2). In these multivariate models, we assessed each risk factor by (a) the number of times the OR is greater than or less than 1 and (b) the interquartile range of the OR (Fig. 4 and Additional file 2: Table S3) to assess their heterogeneity.
The distributions of odds ratios among the selected risk factors across all combinations of SCA analyses (Fig. 3). The red line represents OR = 1, the orange line represents the median ORs, and the blue lines define the IQRs
In Fig. 4, we showed the distribution of the ORs among the selected risk factors. 100% of models that included APOE e4/e4 (ORs = 1.56–8.76), 100% of models that included TBI (ORs = 3.42–14.48), 97% of models with hypertension (ORs = 0.97–4.54), and 93% depression outputs (ORs = 0.87–3.36) are positively associated (OR > 1) with dementia outcomes. Further, higher than high school education categories were all negatively (OR
To assess the robustness of these risk factors (except diabetes) in different dementia subtypes, we compared the OR generated from the no-demographic-adjusted models with the odds ratios from the multivariate models with all six risk factors (Additional file 1: Figure S3). We observed positive correlations between the simple and multi-risk factor models in all dementia subtypes. The highest correlation was in unattributed dementia (R
2 = 0.995, p-value = 2.425e − 10), and frontotemporal dementia showed the lowest correlation (R
2 = 0.694, p-value = 0.002). These findings suggest the robustness of the five risk factors’ associations with dementia outcomes, regardless of model adjustments.
Heterogeneity of risk factors within and across different age groups and dementia subtypes
Next, we compared the ORs for the risk factors within each age group with different justifications (Fig. 5, Additional file 1: Figure S4, and Additional file 2: Table S4). The range of ORs in the age- and gender-adjusted models for APOE e4/e4 in midlife is from 1.57 to 5.09, and in late-life is from 2.77 to 8.78. Similarly, the ranges of ORs for TBI in age- and gender-adjusted models are 6.81 to 13.97 for midlife and 6.92 to 10.15 for late life. In contrast, some risk factors present small differences between dementia subtypes, such as continuous PM2.5 (1 µg/m3). The OR range in PM2.5 (per 1 µg/m3) is in the age- and gender-adjusted model in midlife which is between 0.88 and 1.21, and the range in late life is between 1.13 and 1.17.
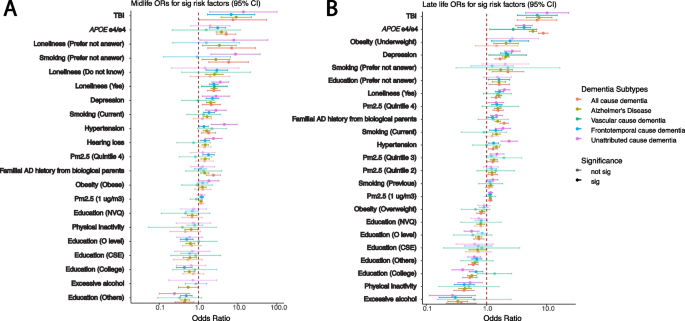
Heterogeneity between different dementia subtypes among significant risk factors identified in age- and gender-adjusted models from the all-cause dementia participants in respective age groups. The ORs and 95% confidence intervals from gender- and age-adjusted models from significant all-cause dementia outputs ranked by the ORs from high to low in midlife (A) and late-life (B) groups. The ORs in the plots are colored by the dementia subtypes, and transparency indicates the significance
There are risk factors that have a significant association (p 5), APOE e4/e4 has significant ORs, from high to low, in AD (5.09 [2.92–8.87]), all-cause dementia (3.85 [2.82–5.24]), and unattributed cause dementia (3.08 [1.93–4.9]) among the midlife participants. Moreover, the APOE e4/e4 ORs are significant among the late-life participants, displaying a different OR ranking and overall larger ORs compared to the midlife group in the age- and gender-adjusted models: AD (8.78 [7.29–10.57]), all-cause dementia (5.90 [5.13–6.78]), unattributed cause dementia (4.23 [3.31–5.40]), vascular dementia (4.19 [3.03–5.79]), and frontotemporal dementia (2.77 [1.12–6.86]). Similarly, intra-group variation in OR rankings also exists in other risk factors, including depression, diabetes, hypertension, loneliness, and TBI.
Heterogeneity of risk factors for unattributed dementia
In the UKB, there are 1189 participants out of 2732 all-cause dementia participants who were not coded into the dementia subtypes (specify how you classified unattributed dementia). We refer to those participants as “unattributed” dementia participants. To understand the risk factors for those participants, we calculated the ORs for those people separately for each age group (Additional file 2: Table S4). Similar to other dementia subtypes, TBI (OR with 95% CI for midlife 6.82 [1.69–27.48] and for late-life OR 6.98 [3.25–14.97]) and APOE e4/e4 genotypes (OR with 95% CI for midlife 3.08 [1.93–4.90] and for late-life OR 4.23 [3.31–5.40]) were among the top risk factors with high odds ratios. Moreover, the rankings of the risk factors in both midlife and late-life groups are similar to the all-cause dementia participants. In midlife, familial AD history from adopted parents, loneliness, depression, smoking, hearing loss, hypertension, and quintile 4 of the PM2.5 are the significant risk factors with ORs greater than 1. In late life, underweight, depression, loneliness, smoking, quintile 4 of the PM2.5, and familial AD history from biological parents have significant odds ratios in all models with ORs greater than 1. Significant education levels have ORs less than 1 in both age groups.
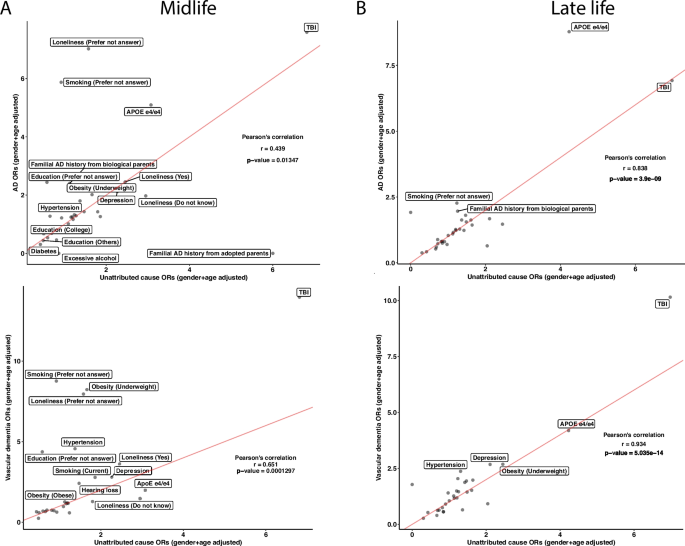
To further investigate the concordance of risk factors between the unattributed dementia participants and known dementia participants, we correlated the ORs of the risk factors between unattributed dementia to each other specific subtype. In the midlife group, the unattributed dementia group had Pearson correlation coefficients of 0.439, 0.651, and 0.703 with vascular dementia, AD, and frontotemporal dementia, respectively (Fig. 6A and Additional file 1: Figure S5A). While most risk factors have similar ORs in the comparisons, some risk factors, such as APOE e4/e4, showed the highest ORs across specifications. In the vascular dementia comparison, the APOE e4/e4 has a higher OR in the unattributed dementia cause group than in vascular dementia. In contrast, it has lower ORs in unattributed dementia when compared to AD. The ORs from unattributed participants significantly correlated with those in AD and vascular dementia participants with Pearson’s correlation coefficients of 0.838 and 0.934, respectively (Fig. 6B and Additional file 1: Figure S5B), whereas a low correlation with the frontotemporal dementia participants with a correlation coefficient of 0.491. In all the late-life comparisons, both TBI and APOE e4/e4 have high ORs. Based on the Pearson correlation results, the unattributed participants are more correlated with participants having frontotemporal dementia in the midlife group and vascular dementia and AD in the life group.
Unattributed cause dementia ORs in all risk factors and their correlations with known cause dementia. We subset the participants with unattributed causes of dementia and reported the ORs on the risk factors in both midlife and late life. We ran correlations on the ORs between the known subtypes of dementia with unattributed causes of dementia in midlife (A) and late-life (B) in AD and vascular dementia. Lastly, we calculated Pearson’s correlation for each comparison and reported the correlation coefficients and the p-values. The red lines in the correlation plots show when the slope is 1. There are N = 131, 67, and 296 participants in the midlife group for AD, vascular dementia, and unattributed cause dementia, respectively, and N = 874, 472, and 873 participants in the late-life group for AD, vascular dementia, and unattributed cause dementia, respectively


)






