Fitness
Heat exposure associated with increased myocardial blood flow | 2 Minute Medicine
1. In this randomized controlled trial, exposure to heat that increased core temperature by 1.5C in healthy participants was associated with nearly double the myocardial blood flow (MBF).
2. Among those with coronary artery disease (CAD), increases in MBF were associated with asymptomatic myocardial ischemia.
Evidence Rating Level: 1 (Excellent)
Study Rundown: A
Climate change increases the risk of exposure to extreme temperatures worldwide. Extreme heat, specifically, is linked to a significant risk of hospitalization and mortality, primarily from cardiovascular events. Heat exposure can lead to vasodilation and higher cardiac output, which could result in ischemia in those with pre-existing CAD. Nevertheless, the degree to which heat exposure causes an increase in MBF is not well characterized. This experimental study sought to assess whether exposure increases MBF and impacts participants across age ranges and CAD status. It was demonstrated that heat exposure that resulted in 1.5C was associated with approximately doubled the MBF among participants regardless of age or presence of CAD. In older participants with pre-existing CAD, some were found to have evidence of asymptomatic myocardial ischemia on imaging. These results were limited to a laboratory setting where blood pressure medications and water were held, which may not reflect real-life situations. Nevertheless, they suggested increased MBF and heat-induced myocardial ischemia as a potential pathophysiological pathway in which heat exposure increases the risk of adverse cardiovascular events in at-risk individuals.
Click here to read the study in AIM
In-Depth [randomized controlled trial]: This was an interventional study to investigate the impact of heat exposure on MBF across age ranges and CAD status. Participants between 18 and 40 years of age (for healthy young adults) and 60 and 89 years of age (for healthy older adults) without cardiovascular, respiratory, neurologic, or metabolic diseases were eligible for inclusion in the ‘healthy’ groups. Exclusion criteria for these groups included smoking within one year, diabetes, body mass index above 35 kg/m2, and uncontrolled hypertension or dyslipidemia. Overall, 61 participants (20 healthy young adults (mean age 28 years), 21 healthy older adults (mean age 67 years), and 20 older adults with CAD (mean age 70)) were heated using a water thermal suit until their core temperature reached 1.5oC above baseline. MBF was measured via positron emission tomography-computed tomography (PET-CT) at baseline and core temperatures 0.5C, 1.0C, and 1.5oC above baseline. Participants were cooled following the last MBF measurement. The primary outcome was the absolute change in global MBF. At baseline, the average MBF was 0.8 mL/min/g (95% confidence interval [CI] 0.7-0.9) for healthy young adults, 0.9 mL/min/g (95% CI 0.9-0.9) for healthy older adults, and 0.9 mL/min/g (95% CI 0.8-0.9) for older adults with CAD. At a core temperature increase of 1.5 oC, global MBF was elevated by 0.8 mL/min/g (95% CI 0.5-1.0) among healthy young adults, 0.7 mL/min/g (95% CI 0.5-0.9) among healthy older adults, and 0.6 mL/min/g (95% CI 0.3-0.8) among older adults with CAD. This elevation translated to a 2.08-fold, 1.79-fold, and 1.64-fold increase from baseline. Regional MBF was also increased across the groups from heat exposure. Although there was no report of anginal symptoms in any participants, PET-CT demonstrated evidence of myocardial ischemia from heat exposure in seven (35%) older adults with CAD, beginning at a core temperature increase of 0.5C from baseline. These results suggested that heat exposure could increase the risk of myocardial ischemia using increased MBF among high-risk individuals with CAD.
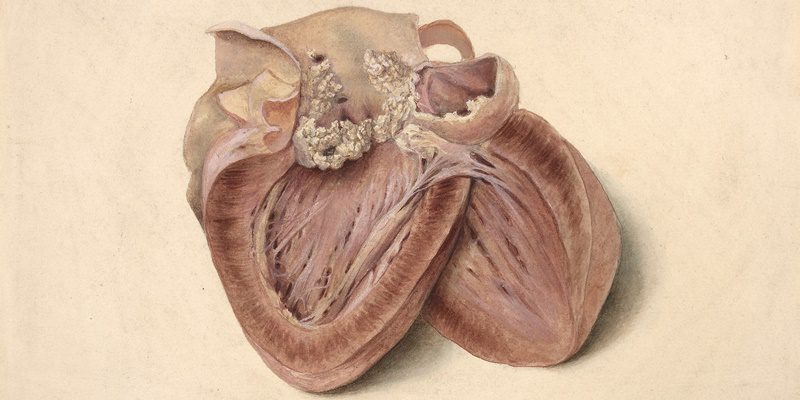
Image: PD
©2024 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.


)






