Addiction is not simply a chronic brain disease and considering it as such can limit treatment options and increase stigma, an extensive research review suggests.
After decades of research, Professor of Developmental Psychopathology Reinout W. Wiers suggests that while in some extreme cases addition can be considered a chronic brain disease, in most cases it should be considered as biased choice.
According to in-depth research examined in new book A New Approach to Addiction and Choice, portraying addiction as a chronic brain disease reduces confidence in the possibility of lasting change, in both the addict themselves and the therapist.
What does science say?
The perception of addiction, in both the scientific community and the general population, has changed over the years.
Until the eighteenth century, addiction was considered to be moral issue that could only be ‘treated’ by punishing the individual. This idea changed over the years and, since the 1990s, addiction has been described as a chronic brain disease, particularly in the biomedical and neuroscience literature.
After a comprehensive literature review, Professor Wiers says that, while there is clear evidence that the brain does change in response to substance use and these changes can indeed make recovery more difficult, this is not enough to class addiction as a chronic brain disease.
Although studies show the brain does change under the influence of addiction, the brain changes during often during the course of a lifetime under many different activities, so the question is the extent to which such changes are unique to addiction and contribute to the maintenance of addiction, as well as the extent to which these adaptations in the brain can normalize again after recovery.”
Reinout W. Wiers, Professor of Developmental Psychopathology
How does addiction impact the brain?
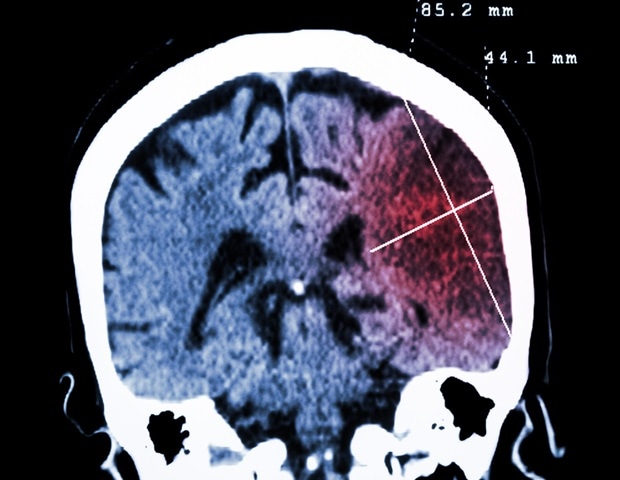
Current neuroscience points to impairments in multiple brain networks. Influential studies show how addiction develops through normal neuropsychological systems that had evolutionarily useful functions.
For example, in the initial stages of substance use, the brain signals an upcoming reward and motivates efforts towards obtaining it, which is the normal ‘wanting’ process. This is a different process from ‘liking’ something and although usually the two coincide, addictive substances (stimulants, opioids, alcohol, nicotine) cause dopamine neural mechanisms (the ‘want’ reaction) to be stronger, even when the person does not like it anymore or even wishes to stop altogether.
Another brain process involved in addiction involves tolerance and withdrawal. The brain adapts to the drug, preparing the body with a counter-reaction which diminishes the euphoric affects and easily leads to escalation – meaning that more of the substance is required to create the anticipated effect.
Other networks involved in addiction include the habit-forming network, the salience network which establishes what individuals consider to be important, and the executive control function network which impacts inhibition and working memory.
“So let there be no mistake: long-term excessive consumption of alcohol has negative effects on the brain in virtually all areas, and the same can be said for other drugs,” Wiers explains.
So why is there a rising tide of dissent against the chronic brain disease model?
Criticisms of the chronic brain disease model
Over the past decade, voices arguing against the chronic brain disease model have grown in volume. They argue that, since the brain is organ undergoing constant change, the fact that there are changes associated with addiction does not in itself prove that addiction is a brain disease.
Wiers points out that the view of addiction as a chronic brain disease, in which relapse is the norm, is heavily based on studies of patients who, for the most part, did relapse after treatment. He argues that many people who struggle with addiction at some point in their lives can overcome the problem, and indeed make full recovery, without ever receiving professional help – a fact that is simply not true of progressive brain diseases such as dementia or Parkinson’s.
Estimates vary by substance, but for the common addictions of alcohol, tobacco and cannabis, less than 10% of people are treated for their addiction.
He explains: “The question, then, is whether the descriptions of heavily addicted people who successfully kick their habit and move on with their lives should be considered the exception or rather as examples of the normal course and that those who fail to quit addiction are the exception and therefore seek professional help. I would argue that based on the epidemiological data, the people whose addiction is best described as a chronic brain disease are the proverbial black swans, not the people who successfully quit.”
Wiers instead suggests considering a model in which addiction is a ‘biased choice’ – a model that embraces the neurobiological findings of altered brain functioning with a developing addiction, without drawing the conclusion that addiction is a chronic brain disease in which choice is no longer possible.
“Nor is the other extreme correct: it does not involve a morally reprehensible choice for the addictive behavior, as the old moral model wanted (chronic drunkenness explained by an exceptional liking of alcohol),” he explains. “In addition, the social and environmental influences that clearly play an important role in risk for addiction can also be modeled to influence choices made.”
Brain disease and stigma
One motivation for moving away from the chronic brain disease model, Wiers suggests, is stigma.
Studies show calling addiction a ‘chronic brain disease’ does reduce the degree to which addicted people are blamed for their problems, but it also leads people to see addicted people as a fundamentally different kind of people, who are dangerous and best kept away from.
In addition, the chronic brain disease perspective has been shown to diminish hope of recovery, both among people struggling with addiction themselves and those around them, including their treatment providers.
He also points to studies suggesting this perspective leads to an ‘all or nothing’ approach to recovery, even when reduction in use can be beneficial. Looking at a recent meta-analysis of research on the effectiveness of AA-like abstinence-based treatment, it yielded slightly better abstinence outcomes than other treatments but was also more likely to lead to full relapse if abstinence is not sustained.
“The perspective of addiction as a chronic brain disease may hold true for a small group of severely addicted people who, despite repeated attempts, are unable to discontinue their addiction. In these exceptional cases it may also help to accept the diagnosis of a chronic addiction rather than despair about it, but for the vast majority of addicted people the image of people with chronic brain disease is neither justified nor useful,” he explains.
According to the ‘biased choice’ alternative, people make decisions based on predictions of the consequences of our actions, and this process can be influenced by therapy and by varieties of cognitive training, either computerized or in the form of mindfulness meditation.
“The bottom line is that the evidence that we can intentionally influence our behavior is empirically strong: it is supported by a wealth of studies, and the effects are strongest for the indirect effects, on later behavior rather than on the choice at the moment,” he concludes.
Wiers suggests this ability to steer behavior towards future goals is vital in tackling contemporary addictive behaviors (including smartphone use, eating meat and using fossil fuels) and working towards climate goals, for example: “Our ability to foresee long-term consequences of our actions is a crucial ability to stimulate, be it to overcome an addiction or to change our behavior for the future of our planet.”
Source:
Journal reference:
Wiers, R. W. (2024). A New Approach to Addiction and Choice. Routledge. doi.org/10.4324/9781032634548.


)






